Micro-TESE surgery is defined as examining and sampling testicular tissue under microscopy to search for sperms. This operation is used in males who have not sperm cells in their ejaculate (azoospermia) due to a sperm production disorder (Non-obstructive azoospermia). Micro-TESE operation is not indicated in men who have normal sperm production but not sperm ejaculation due to an obstruction, since normal sperm production occurs everywhere in the testicles of these men, and using microscopy to search for sperms is irrelevant. Spermatozoa can be easily recovered by removing a tissue sample from anywhere in the testis or by needle aspiration of fluid-tissue from the testicular tissue (TESA).
What type of anesthesia is used for the micro-TESE procedure?
General anesthesia is preferable for micro-TESE, depending on the overall health condition of the patient. Because it is a highly detailed operation conducted under microscopy and requiring utmost concentration, general anesthesia is the best option for both the patient’s comfort throughout a relatively long procedure and ensuring the uninterrupted concentration of the doctor performing the procedure. General anesthesia is also optimal to prevent any psychological distress to the patient during this long procedure. Unhindered focus and concentration of the operator examining the tissues during micro-TESE surgery are crucial. Therefore, general anesthesia is used unless precluded by very unique circumstances.
What is the difference between TESE and micro-TESE?
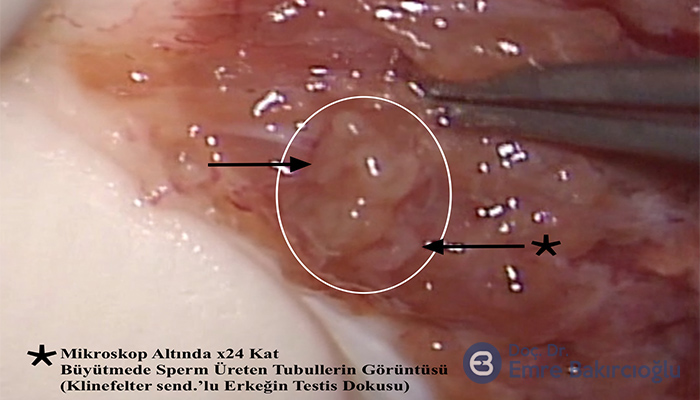
Unlike the conventional TESE procedure, the testicle is completely opened by a single horizontal incision. Sperm-producing tubular structures in the inner and deep regions of the testicle are reached and examined under microscopy with 20 to 25x magnification. The microscope we use can achieve up to 40x magnification. In some patients, high magnification helps us with the very small differences in the diameters of tubules, making it easier to select the ones that produce sperms. The probability of success is much higher with micro-TESE, compared to conventional TESE which involves multi-biopsy from tissues with dilated or close-to-normal tubular structures. The micro-TESE operation makes it possible to harvest a higher number of sperms from less testicular tissue. In azoospermic (NOA) males, the loss of testicular tissue is up to 70-fold less with the microsurgical method, compared to multi-biopsy, which minimizes injury to testicles from the procedure and the effects of testosterone secretion.
Another benefit of micro-TESE, which is conducted under microscopy, is that the vascular structure of the capsule enveloping the testicular tissue can be more clearly observed with a microscope, allowing incision without damaging the vessels supporting the testicles. This important benefit minimizes potential postoperative complications. Studies comparing the testosterone levels of males that underwent micro-TESE vs multi-biopsy have shown that the testosterone levels were comparable to the preoperative levels with micro-TESE. However, the preoperative testosterone levels may be low in some azoospermic males with impaired sperm production. It is advisable to identify these males before micro-TESE, and elevate their testosterone to normal levels before the operation, and ensure regular postoperative follow-up of these patients.
What would be your advice to patients before and after micro-TESE?
Because micro-TESE is conducted under general anesthesia, the patients are advised to withhold foods and drinks on the operation day and come to the hospital with an empty stomach. General anesthesia is preferred for the comfort of both the patient and the doctor and their team. Micro-TESE under local anesthesia is not advisable, unless exceptional circumstances require it, considering that the patient will have to remain still on the surgical table for an extended period of time; the patient may experience psychological distress during the operation, and it would be less likely for the doctor to be distracted when operating under general anesthesia. After micro-TESE, the patient is kept under observation in the ward for some time after they regain consciousness from anesthesia and discharged following final checks and controls to rest at home. Because the patient was under general anesthesia, driving vehicles after leaving the hospital is not advisable. The patient should be with the company for the surgery.
The patient will not need to remain in the bed for recovery; however, because this is a delicate procedure, it is advisable to reduce normal daily activity for a couple of days. The dressing of the incision site needs to be replaced 48 hours after surgery. The patient is allowed to take a shower after three days. Because the stitches are self-absorbing, they need not be removed.
The patients are advised to use tight underwear or jockstraps for a week to 10 days after surgery. Demanding physical activities, sports and coitus should be avoided for a week to 10 days after surgery.
For which type of azoospermic patients is micro-TESE particularly important?
Males with the Klinefelter Syndrome, a genetic disorder that affects one in every 500 males in the world, suffer from infertility due to smaller-than-normal testicle size (2-3 mL), reduced testosterone levels, and absence of sperms in the seminal fluid (azoospermia).
A 50% rate of success has been achieved in harvesting sperms by micro-TESE from males with the Klinefelter Syndrome. Micro-TESE also has a high rate of success in harvesting sperms in males with azoospermia secondary to mumps orchitis, men who had orchiopexy operation, or in males with germ cell aplasia (Sertoli-Cell-Only). However, the experience of the urologist performing the micro-TESE procedure is another factor in the rate of success.
After having sperms harvested by micro-TESE, how long must a patient wait repeat the procedure, and how likely is it for sperms to be harvested again in the second operation?
A patient must wait at around 6 months to repeat the micro-TESE procedure. The probability of harvesting sperms a second time by micro-TESE is approximately 80 to 90%, depending on the characteristics of the patient and his testicles.
Would you recommend a patient to undergo micro-TESE a second time, if no sperms could be harvested in the first procedure?
In males with azoospermia due to production impairment, drug treatment is not possible, except in the case of hormonal deficiency, i.e. hypogonadotropic hypogonadism. Today, micro-TESE is the most advanced technique for harvesting sperms from testicular tissue in azoospermic males with elevated FSH values. However, the experience of the operating surgeon, the technical capabilities, and the experience of the embryology laboratory are strong determinants of success.
The studies have shown that the probability of finding sperms may be as high as 45% in the next operation, where nor sperms could be harvested from 3 or 4 samples previously removed, randomly and without substantial microscopic magnification or detailed examination (Tsijumura A et al. J Urol 2006). Accordingly, repeating the search for sperms by micro-TESE may be advisable, after no sperms could be harvested by multi-TESE or micro-TESE performed using suboptimal technological means. However, if sperms could not be harvested by micro-TESE performed properly by an experienced specialist, the probability of finding sperms in a second run remains similarly low. Personally, I do not advise my patients to repeat micro-TESE at a later date, if no sperms could be harvested in the first try (excluding exceptional cases, e.g. pathological examination reports presence of matured sperms). I could say, from my experience, that the probability of finding sperms at a second micro-TESE that I perform, in patients that underwent micro-TESE at another clinic and no sperms could be harvested, would be around 15 to 20%.
How many times can a patient undergo micro-TESE?
Because very small samples are removed from the testicular tissue and utmost care is exercised so as not to damage the vascular structure when making the incision, damage to the testicles would be far less than with multi-biopsy TESE. And the extent of damage that the testicles would suffer from this special operation depends on the size of the patient’s testicles, preoperative total testosterone levels, and previous history of TESE procedures (the technique of the TESE procedure). Therefore, it would be best to examine the patient thoroughly and inform them based on patient-specific data.
Is it possible to harvest sperms by PESA / MESA in males with impaired sperm production?
No. These methods are indicated in males with obstructive azoospermia. Because azoospermia is not caused by an anatomic obstruction, it is not possible to harvest sperms from the epididymis, i.e. the ducts, or directly from the testis in these males.
What is the likelihood that the sperms that had been harvested by micro-TESE and frozen would be viable after thawing for microinjection therapy?
The studies indicate average viability of 50% for thawed sperms. Although nearly 90% of sperms harvested from testicular tissue are vital (alive), only 5% of them are motile. Therefore, sperm motility, which is a key marker of sperm viability after thawing, is significantly reduced. However, if a high number of sperms were harvested, usually there should be no problem finding a sufficient number of motile sperms for ICSI after thawing. The micro-TESE procedure enables a higher number of sperm than the other sperm retrieval technique so that frozen thaw testicular sperm quality is better. Therefore, in most clinics in Europe and around the world, azoospermic males first undergo sperm investigation in the testicular tissue and their sperms are frozen. Afterward, their spouses undergo ICSI. My approach, in this case, is to explain the benefits and drawbacks of the procedure to the patient and his spouse before deciding on preparing for IVF, before using the freeze and thaw method, and reach a joint decision after hearing their views.
